"Buy discount ventolin online, asthma symptoms from anxiety".
By: G. Sinikar, M.A., M.D., M.P.H.
Co-Director, University of California, Merced School of Medicine
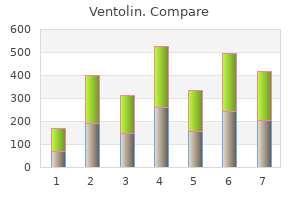
It should not be used in osteoporotic asthma definition 6 careers order cheap ventolin online, elderly patients or those with comminution secondary to a higher loss of reduction asthma symptoms when to go to hospital purchase genuine ventolin. An incision is made over the radial styloid and a K-wire is manually inserted into the fracture site asthma icd 9 order ventolin with visa. The wire is levered distally to correct the dorsal angulation and advanced proximally using power into cortical bone. Using the modified technique, a third pin is placed retrograde using power, starting at the radial styloid and pro- ceeding into the ulnar cortex of the radius proximal to the fracture line. Alternatively, the pins may be bent using two needle drivers and left outside the skin. A small incision is placed over the interval between the fourth and fifth dorsal compartments. The index metacarpophalangeal joint is flexed to protect the sagittal band and first dorsal interosseous aponeurosis. The metacarpal drill guide is placed on the radial base of the index metacarpal at the flare of the metaphysis. An incision is made over the second metacarpal base, with reflection of the first dorsal interosseous muscle and radial sensory nerve terminal branches. Diagram showing placement of fixator pins in the shaft of the index and the base of the index and long metacarpals. Proximal Pin Placement and Frame Construction A 4- to 5-cm incision is made over the radial forearm, proximal to the first dorsal compartment musculature, through skin and subcutaneous tissue, avoiding the lateral antebrachial cutaneous nerve branches. The fracture should be reduced, and the pins placed parallel to the metacarpal pins to facilitate alignment of the fracture. The proximal pin should be placed bicortically, just distal to the tendon of the pronator teres. The incisions are closed using nylon suture, ensuring no tension is on the skin at the pin sites. Incision over the radial forearm demonstrating the radial sensory nerve branch deep to the fascia. The wrist is placed for a lateral fluoroscopic view, and a marker is used to determine the level of incision halfway between the radiocarpal joint and the fracture. This pin should be placed parallel to the first pin in both planes, with the starting point halfway between the radiocarpal joint and the fracture. The two proximal radius pins are placed using the technique described for placement of a bridging external fixator. Determine comminution and supplement fixation with external or internal fixation as necessary. Make skin incisions for pin placement to avoid sensory nerves, tendons, and crossing veins. Obtain adequate exposure of the radial sensory branch at forearm and hand to avoid injury. Do not leave pins more than 1 to 2 mm out of the cortex, and keep all pins extra-articular. If placing the proximal metacarpal pin in metaphyseal bone, ensure that three cortices are penetrated. Subcutaneous pins are more costly to remove, because that requires a second procedure, but they have a lower infection rate. Encourage early range of motion of the fingers, elbow, and shoulder whenever possible.
Patients usually present with pain in the antecubital fossa asthma zone system trusted 100 mcg ventolin, especially with resisted flexion and supination asthma symptoms dogs purchase ventolin uk. The surgeon should discuss with the patient that complete distal biceps tendon ruptures are not usually associated with residual pain but rather loss of flexion (30%) and supination (40%) strength asthma symptoms mild moderate severe cheap 100mcg ventolin. Partial biceps tendon ruptures and ruptures at the myotendinous junction are treated in a similar manner. The patient should proceed to strengthening when full painless range of motion is obtained. Operative intervention is considered when nonoperative management fails for partial ruptures. Patients should be counseled that pain is more of a predominant complaint with these partial injuries. Some authors have stated that greater than 8 weeks is chronic and that a graft is needed in these situations. However, we have been able to primarily repair distal biceps tendon ruptures out to 3 months. The biceps brachii, like the pectoralis major, has a significant ability to stretch back out over time. The surgeon should discuss with the patient that a more chronic rupture might require graft and should discuss the type of graft to be used. Semitendinosus (either autograft or allograft),16 Achilles tendon allograft13 (with the bone plug inserted into the radial tuberosity or just soft tissue repair), flexor carpi radialis autograft,9 and fascia lata6 have been described. Any of the techniques of radial tuberosity fixation described in the acute section can be used. Positioning the patient is placed in the supine position on an armboard with a sterile tourniquet on the upper arm. Classic two-incision techniques had complications such as heterotopic ossification and posterior interosseous nerve palsy. Therefore, single-incision anterior approaches were developed with various methods of fixation, including suture anchors, interference screws, and the EndoButton. The lateral antebrachial cutaneous nerve and superficial radial nerve are identified and protected. This can be accomplished by flexing the elbow and using a retractor to lift the skin of the distal arm for exposure. Protect and isolate the lateral antebrachial cutaneous nerve and the brachial artery. In that case, an incision can be made medially along the distal aspect of the arm. The goal is to create a locking stitch proximally and allow about 1 cm of the distal biceps tendon to be unlocked. The two sutures extending from the tendon stump are then passed through the two central holes of the EndoButton. Alternatively, one suture from the tendon can be passed through one of the central holes of the EndoButton and then back through the other central hole and the knot is then tied, thus placing the knot between the EndoButton and the tendon stump. Passing sutures (kite strings) are placed in the other two holes of the EndoButton. The radial tuberosity is exposed, and a burr is used to create an oval cortical window roughly the same dimension as the distal tendon stump. Two small Bennett retractors can be placed on either side of the radial tuberosity.
Purchase ventolin 100 mcg free shipping. Exercise-Induced Asthma (Health Short).
Skip nodules are tumor foci not in continuity with the main tumor mass that form outside the pseudocapsule asthma differential diagnosis buy ventolin 100mcg line. The growth plate asthma treatments buy ventolin with amex, although not invaded by the tumor in this case asthma symptoms status epilepticus buy discount ventolin 100mcg on line, is not considered an anatomic barrier to tumor extension, probably because of the numerous vascular channels that pass through the growth plate to the epiphysis. However, the articular cartilage is an anatomic barrier to tumor extension and very rarely is directly violated by a tumor. Although gross involvement of the epiphysis and medial cortical breakthrough and soft tissue extension are evident, the articular cartilage is intact. This phenomenon allows intra-articular resection of high-grade sarcomas of the distal femur in most cases. The tumor does not penetrate, looking in a clockwise direction, the lateral intermuscular septum, the adductor compartment, and the aponeuroses of the sartorius and rectus femoris muscles. It is only at a later stage that the walls of the compartment are violated (either the cortex of a bone or aponeurosis of a muscle), at which time the tumor breaks into a surrounding compartment. Typical anatomic barriers are articular cartilage, cortical bone, and fascial borders. Sarcomas are defined as intracompartmental if they are encased within an anatomic compartment. Most bone sarcomas are bicompartmental at the time of presentation; they destroy the overlying cortex and extend directly into the adjacent soft tissues. Joint involvement in sarcoma is uncommon, because direct tumor extension through the articular cartilage is rare. Metastatic Bone and Soft Tissue Sarcomas Unlike carcinomas, bone and soft tissue sarcomas disseminate almost exclusively through the blood. Hematogenous spread of extremity sarcomas is manifested by pulmonary involvement in the early stages and by bony involvement in later stages. Abdominal and pelvic soft tissue sarcomas, on the other hand, typically metastasize to the liver and lungs. Low-grade soft tissue sarcomas have a low (under 15%) rate of subsequent metastasis, whereas high-grade lesions have a significantly higher (over 20%) rate of metastasis. Ewing sarcoma of the distal two thirds of the femur (A) and osteosarcoma of the proximal tibia (B). Most high-grade bone sarcomas are bicompartmental at the time of presentation (ie, they involve the bone of origin as well as the adjacent soft tissues). Plain radiograph of the proximal femur revealed direct invasion through the cortical bone with a pathological fracture of the lesser trochanter (arrows). In surgery, exploration of the sciatic nerve revealed direct tumor involvement with extension under the epineural sheath. Extension of an osteosarcoma of the distal femur to the knee joint along the cruciate ligaments (arrow points to tumor); the articular cartilage is intact. Knee joint extension of a high-grade sarcoma of the distal femur is a rare event, necessitating extra-articular resection (ie, en bloc resection of the distal femur, knee joint, and a component of the proximal tibia). Most patients with high-grade primary bone sarcomas, unlike soft tissue sarcomas, have distant micrometastases at presentation; an estimated 80% of patients with osteosarcomas have micrometastatic lung disease at the time of diagnosis. For this reason, in most cases, cure of a high-grade primary bone sarcoma can be achieved only with systemic chemotherapy and surgery. Because of that difference in metastatic capability, the role of chemotherapy in the treatment of soft tissue sarcomas and its impact on survival are still matters of some controversy. Prognostic factors for soft tissue sarcomas include grade, tumor size, depth, age, margin status, location (proximal vs. Staging Staging is the process of classifying a tumor, especially a malignant tumor, with respect to its degree of differentiation, as well its local and distant extent, to plan the treatment and estimate the prognosis.
The posterior aspect of the distal femur is a classic location for parosteal osteosarcomas asthma definition who buy ventolin canada, and that diagnosis should be considered for any sclerotic lesion in that location asthma treatment 4 addiction ventolin 100mcg discount. In contrast to osteochondromas asthma treatment without medicine order ventolin cheap online, the medullary canal of the bone is not contiguous with that of the tumor. Specimen shown illuminated with tetracycline fluorescence, which demonstrates minimal medullary tumor extension through the posterior cortex. There are parallel or intersecting osseous trabeculae (arrows) that may be either lamellar or woven-type bone matrix. The intervening fibrocollagenous tissue is composed of bland, widely-spaced fibroblastic cells. Pain, which indicates active growth, is an ominous sign of a central cartilage lesion. Radiographic Findings Central chondrosarcomas have two distinct radiological patterns. This type is difficult to diagnose on plain radiographs and may go undetected for a long period of time. Peripheral chondrosarcoma is easily recognized as a large mass of characteristic calcification protruding from a bone. Correlation of the clinical, radiographic, and histologic data is essential for accurate diagnosis and evaluation of the aggressiveness of cartilage tumor. In general, proximal or axial location, skeletal maturity, and pain point toward malignancy, even though the cartilage may appear benign. The sites of origin and the fact that chondrosarcomas tend to be low-grade often make them amenable to limb-sparing procedures. The four most common sites are the pelvis, proximal femur, shoulder girdle, and diaphyseal portions of the long bones. Variants of Chondrosarcoma There are three less-common variants of classic chondrosarcoma. Clear cell chondrosarcoma, the rarest form of chondrosarcoma, is a slow-growing, locally recurrent tumor resembling a chondroblastoma but with some malignant potential that typically occurs in adults. The most difficult clinical problem is early recognition; it often is confused with chondroblastoma. Mesenchymal chondrosarcoma is a rare, aggressive variant of chondrosarcoma characterized by a biphasic histologic pattern, ie, small, compact cells intermixed with islands of cartilaginous matrix. This tumor has a predilection for flat bones; long tubular bones rarely are affected. Grading and Prognosis Chondrosarcomas are graded 1, 2, and 3; most are either grade 1 or grade 2. Ten-year survival rates among those with peripheral lesions are 77% with 32% among those with central lesions. The multiple forms of benign osteochondromas or enchondromas have a higher rate of malignant transformation than the corresponding solitary lesions. Ewing Sarcoma Ewing sarcoma is the second most common bone sarcoma of childhood; it is approximately one half as common as osteosarcoma. The lesion is characterized by poorly differentiated, small, round cells with marked homogeneity. The clinical and biologic behavior is significantly different from that of spindle cell sarcomas. Within the past 2 decades, the prognosis of patients with Ewing sarcomas has been improved dramatically thanks to a combination of adjuvant chemotherapy, improved radiation therapy techniques, and the select use of limited surgical resection. Microscopic Characteristics the histologic spectrum of chondrosarcomas varies tremendously. High-grade examples are easy to identify, whereas certain low-grade tumors are exceedingly difficult to distinguish from chondromas.