"Generic 0.5 mg cabgolin with amex, treatment of pneumonia".
By: Y. Surus, M.A., M.D.
Associate Professor, UT Health San Antonio Joe R. and Teresa Lozano Long School of Medicine
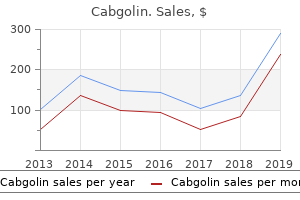
Kulmala and colleagues (1996) reported 92% erectile function preservation among patients with ischemic priapism reversed in less than 24 hours symptoms job disease skin infections generic 0.5mg cabgolin fast delivery, but only 22% preservation of erectile function among men with priapism lasting longer than 7 days medicine lookup cheap cabgolin 0.5mg. A standard protocol of aspiration and phenylephrine injection was performed; shunting for failure of medical management was performed in 28% medicine for pink eye buy cabgolin in united states online. In patients in whom priapism was reversed, spontaneous erections (with or without use of sildenafil) were reported in 100% of men when priapism was reversed by 12 hours; 78% when reversed by 12 to 24 hours; and 44% when reversed by 24 to 36 hours. The International Society for Sexual Medicine Standards Committee (expert opinion) stated that shunting is to be considered for ischemic priapism events lasting 72 hours or less. Consideration should be given to foregoing a shunt in priapism events lasting longer, in particular when cavernous thrombosis is evident and no blood can be aspirated from the corporal bodies (Pryor et al, 2004; Mulhall, 2006). Shunt procedures are subdivided on the basis of anatomic location on the penis (Lue and Pescatori, 2006). Percutaneous distal shunting is less invasive than open distal shunting and can be performed with local anesthetic in the emergency department. Brant and associates (2009) describes 13 men with priapism durations longer than 24 hours (in 6 of 13, other distal or proximal shunt procedures had failed). All T shunts were performed after penile anesthetic block; in 12 of 13 patients, the priapism was successfully reversed by initial intervention. The authors recommend discharge home if the penis remains flaccid for 15 minutes (Brant et al, 2009). If erection returns or persists, a second T shunt is recommended on the opposite side of the meatus. Burnett and Pierorazio (2009) have described a similar technique to resolve ischemic priapism refractory to first-line interventions. Their procedure, known as the corporal snake, is a modification of the Al-Ghorab corporoglanular shunt. The penis is made flaccid by repeated manual compression and release; the glans skin is then approximated with 4-0 chromic sutures; a urethral catheter is placed, and lightly compressive dressing is applied to the genitalia. Segal and associates (2013) retrospectively reviewed the Johns Hopkins Hospital experience with the corporal snake maneuver. Ten patients with ischemic priapism with a mean duration of 75 hours (range 24 to 288 hours) refractory to medical intervention and simple distal shunting (Winter or Ebbehoj) were treated surgically with the corporal snake maneuver; in 8 the priapism resolved, and they had no postoperative recurrence during 6-month follow-up. In 2 patients the priapism did not respond; they were treated by insertion of inflatable penile implant at time of presentation. Complication rates were significant (20%); complications Chapter28 Priapism 685 A B A B Figure 28-8. The distal cavernoglanular shunt procedure is depicted by the transglanularplacementofalarge-boreneedleorangiocatheterinthedistalglansandcorpus cavernosum. Afterexcision of a 5-mm circular core of distal tunica albuginea, a 7/8 Hegar dilator is inserted down eachcorporalbodythroughthetunicawindow. Inboththepercutaneoustechniquesdeoxygenated blood is milked out of the open wounds; once bright red blood is seen, the skin is closed, leaving the deeper incision of the open fistula. Zacharakis and colleagues (2014b) described the efficacy and outcomes of combining the T shunt (Brant et al, 2009) with the corporal snake maneuver in 45 patients. The combined distal surgical technique was successful in resolving the acute priapism if duration was less than 24 hours but had limited efficacy in cases of priapism exceeding 48 hours. Corporal needle biopsies were performed in each patient and documented smooth muscle necrosis, worsening as a function of time and uniform in all men with more than 48 hours of ischemia. The authors (Zacharakis et al, 2014b) conclude that the cutoff for reversing ischemic priapism in the hopes of preserving future erectile function is 48 hours.
Diseases
- Achard syndrome
- Mental retardation short stature ocular and articular anomalies
- Fetal thalidomide syndrome
- Rudd Klimek syndrome
- Staphylococcus epidermidis infection
- Fetal hydantoin syndrome
- Spinal muscular atrophy type 1
- Mucolipidosis type 4
- Megacystis microcolon intestinal hypoperistalsis syndrome
Hormonal contraceptives (oral symptoms with twins purchase generic cabgolin canada, subcutaneous medications of the same type are known as order cabgolin discount, injectable) modulate E to prevent ovulation symptoms in early pregnancy cheap cabgolin 0.5mg with mastercard. This synergistically lowers bioavailable T and may contribute to sexual side effects (Coenen et al, 1996). Specific changes reported in some women using hormonal contraception include decreased sexual desire, atrophy and pain in the labia and genital tissues, decreased intercourse frequency, and decreased orgasmic function. Some women tolerate hormonal contraception without discernible perturbation of their sexual life; several studies have reported no objective or subjective changes in sexual function in women using hormonal contraceptives (Shirtcliff et al, 2002; Greco et al, 2007; Flyckt et al, 2009; Kovalevsky et al, 2010; Lee et al, 2011). However, some women may be particularly sensitive to the androgen-lowering effects of hormonal contraception (Bancroft and Graham, 2011). Use of an agent with androgenic effects may be of benefit in women with sexual issues related to hormonal contraception (Davis et al, 2013). Discomfort may stem from personal embarrassment or shame about sexuality, fear of embarrassing the provider, a sense that nothing can be done, a sense that sexual dysfunction is not a medical problem and/or not a significant problem to be addressed, or a simple lack of time during health care encounters (Nicolosi et al, 2006b). Unfortunately, many providers also have difficulty initiating conversations about sex for reasons similar to those given by patients (Merrill et al, 1990; Tsimtsiou et al, 2006). Many providers also report a lack of training in how to appropriately address sexuality with patients (Parish and Rubio-Aurioles, 2010; Shindel et al, 2010). The bulbospongiosus and ischiocavernosus muscles, located superficially and Chapter32 SexualFunctionandDysfunctionintheFemale 752. This may result in glans clitoris atrophy (A), erythema of the minor vestibular glands(B),andlimitedrobustperiurethraltissue(D). These observations indicate a substantial potential for a disconnect between subjective and objective sexual arousal in women. In a forensic sense, these data may explain why some women experience genital responses such as vaginal lubrication in the context of nonconsensual sexual activity. Various theories have been advanced on how this may be an evolutionary adaption to ensure adequate lubrication (and hence reduced risk of vaginal trauma) even in the context of undesired sexual activity (Chivers and Rosen, 2010). Despite this biologic observation, interpersonal and psychosocial factors are tremendously important in the sexual response for women. Psychological and emotional responses modulate how a woman expresses her sexuality and how she responds to sexual initiation from a partner. Other reports have confirmed the primacy of the marital relationship and general health over menopausal status as predictors of satisfying sexual function (Avis et al, 2000; Dennerstein et al, 2005). Historically these issues have been considered central to sexuality in women and of lesser import in men; one may hypothesize that the dearth of biomedical understanding about female sexuality (and subsequent dearth of nonpsychological treatment options) may play a role in fostering this concept. Chapter32 SexualFunctionandDysfunctionintheFemale 753 screeners, follow-up with open-ended questions will likely produce more nuanced and informative responses (Kingsberg and Althof, 2009). Allowing the woman to voice any concerns she has about her sexual life and satisfaction is one of the most basic but critical interventions that providers may make on behalf of sexual wellness. The opportunity to discuss sexuality issues with a professional may substantially decrease sex-related distress (Goldstein and Alexander, 2005). Additional advice on taking a sexual history is available in the online supplement. Serum and Other Laboratory Studies in the Evaluation of Sexual Wellness the role of serum studies in evaluation of female sexual wellness is controversial (Goldstein and Alexander, 2005; Basson et al, 2010b). Serum chemistry, lipids, and glycosylated hemoglobin should be assayed, as these are low-risk tests for common problems potentially relevant to female sexual function. Assessment of sex steroids, particularly serum E and T, should be considered if there is concern for significant endocrinopathy (Utian et al, 2008; Kingsberg, 2009). Serum T testing is controversial because of questions of relevance and precision of results; most widely available assays for T are not precise at the levels typical in women (Stanczyk et al, 2003; Bancroft and Graham, 2011).
Cabgolin 0.5mg with visa. Don't Ignore These Early Symptoms of Breast Cancer.
Partial erection spontaneously resolved 4 days after diagnostic evaluation treatment of scabies order cabgolin 0.5mg mastercard, with the patient reporting normal erections 2 weeks later treatment xanax withdrawal buy cheap cabgolin 0.5 mg line. The authors hypothesized that in patients with blunt penile and perineal trauma treatment 5th metatarsal base fracture 0.5mg cabgolin mastercard, an arteriolacunar fistula forms; these fistulae, unlike arteriovenous communications, may spontaneously resolve because the less rigid walls of the lacunae are prone to spontaneous thrombosis. Although the site of perineal trauma may have hematoma, spreading of the hematoma to the shaft should raise suspicion of rupture of tunica albuginea; this would be highly unusual in blunt perineal (straddle) injury. Because there is no restriction of venous outflow, erection is partial and bendable. Patients do report additional engorgement with sexual stimulation, with return to partial erection after climax. Color Doppler ultrasonography of the penis and perineum is recommended in the evaluation of priapism when the history or examination findings suggest penile trauma (A). Conservative measures include ice applied to the perineum and site-specific compression. Repeated aspirations, injection, and irrigation with intracavernous sympathomimetics have no role in the treatment of nonischemic priapism. Patients demanding immediate relief can be offered selective arterial embolization. The pathognomonic arteriographic finding is an arteriolacunar fistula; a characteristic intracavernosal coneshaped blush of contrast is seen at the site of the cavernous artery or arteriole laceration. Selective internal pudendal catheterization and subsequent embolization have been reported with various agents: microcoils, polyvinyl alcohol, N-butylcyanoacrylate, gel-foam, and autologous blood clot (Kuefer et al, 2005). Autologous blood clot has a low risk of foreign body reaction, or antigenicity; it is a temporary occlusive agent and should permit recanalization of the cavernous artery (Park et al, 2001). Currently this intervention is reserved for patients who do not wish to pursue expectant management or who are poor candidates for angioembolization. It is also reserved for patients who refuse the procedure; for patients in places where technology is not available; and for patients in whom angioembolization has failed (Ji et al, 1994; Berger et al, 2001; Mulhall, 2006). Normal postembolization erectile function has been reported in 75% to 86% of patients (Cakan et al, 2006; Numan et al, 2008). It should be noted that a single treatment of embolization carries a recurrence rate of 30% (Ciampalani et al, 2002; Gandini et al, 2004; Ozturk et al, 2009). Other reported adverse effects include penile gangrene, gluteal ischemia, purulent cavernositis, and abscess of the perineum (Hakim et al, 1996; Sandock et al, 1996). Puppo and colleagues (1985) compared perineal duplex ultrasound and selective internal pudendal arteriography, showing excellent sensitivity of ultrasound in detecting arteriolacunar fistulae that were seen angiographically (12 of 12 cases). Several reports have described combined ultrasound-guided compression with selective arterial embolization to increase success rates in the treatment of nonischemic priapism (Hatzichristou et al, 2002; Bartsch et al, 2004; Cakan et al, 2006). Any intervention must follow a comprehensive discussion with the patient regarding risks and benefits of any of the procedures advocated by the clinician. In cases of longstanding arterial priapism in which a pseudocapsule around the fistula has developed, surgical ligation has been reported to be successful. In ischemic priapism there are time-dependent changes in the corpora with progressive hypoxia, hypercarbia, and acidosis. Treatment for ischemic priapism is administered in stepwise manner: decompression of the corpora by needle aspiration, injection and irrigation with a dilute sympathomimetic drug, surgical shunting, and consideration of immediate penile implant in refractory cases. A history of blunt trauma (a straddle injury) or an iatrogenic needle injury to the penis is common. Urologists intervening to treat priapism should use standardized questionnaires to document the history of the prolonged erection: onset, trauma, medical history of blood dyscrasias, use of illicit substances, prior events, prepriapism erectile function, recurrence after each intervention, and recovery of erectile function.
Achiote (Annatto). Cabgolin.
- Diarrhea, diabetes, fevers, hepatitis, sunburn, and other conditions.
- What is Annatto?
- Are there safety concerns?
- How does Annatto work?
- Dosing considerations for Annatto.
- Are there any interactions with medications?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96073